(as of April 20, 2020 4:59 am GMT+0000 - Details) + Add To Wish List
(as of April 20, 2020 4:59 am GMT+0000 - Details) + Add To Wish List
This is the break that Cynthia has been waiting her whole life for. It’s her first real shot at fame. A chance to break out of the small club scene takes her career to the next level. That’s why her producer, one of the most prestigious on the New York music scene, has invited her [More]
(as of April 19, 2020 5:01 pm GMT+0000 - Details) + Add To Wish List
If Ray Bradbury and Douglas Adams collaborated on writing, they’d present something like this incredible collection of science fiction short stories. Have you ever wondered what an alien abduction is like from the alien’s viewpoint? Can a dying woman receive solace and comfort from a machine? What would it be like to fall into the hands of a get-rich-quick [More]
(as of April 19, 2020 9:02 pm GMT+0000 - Details) + Add To Wish List
Saint Augustine * * *Download for FREE on Kindle Unlimited + Free BONUS Inside!* * * Read On Your Computer, MAC, Smartphone, Kindle Reader, iPad, or Tablet. Although he was born in what was considered the backwaters of the Roman Empire, Saint Augustine of Hippo has long been renowned for his early religious and philosophical [More]
(as of April 19, 2020 5:01 pm GMT+0000 - Details) + Add To Wish List
Young man goes on vacation with his girlfriend, her mother and her mother’s best friend.Chapter 7 – Carla manipulates Ethan into a day at the beach Intended for adult readers only! tags: vacation – tempting – seduction – teasing – cunnilingus – sex on the beach – blow job – swallowing – public sex – [More]
(as of April 19, 2020 9:00 am GMT+0000 - Details) + Add To Wish List
A child born of violence, a woman with a prophecy, and a personal vendetta that will mark their fate… Robbie MacDonald wished he was never born. His father’s forceful ways tormented his very existence. Without a feeling of belonging he decides to leave the isle of Skye and pursue a future as a mercenary in [More]
(as of April 20, 2020 5:01 am GMT+0000 - Details) + Add To Wish List
Get ONE hot BWWM romance Novel and THREE steamy BWWM romance short stories or enjoy over 80,000+ words of reading inside! Love Is On Our Side- BWWM and Billionaire Romance NovelA Special Day– Playboy BWWM RomanceA Love so Strong– BWWM Basketball RomanceTHE ROMANTIC ESCAPADE – BWWM Threesome MFM Werebear Shifter Romance WARNING: This book contains [More]
(as of April 19, 2020 1:00 pm GMT+0000 - Details) + Add To Wish List
What if there’s a hidden dimension to Donald Trump; a sensitive, poetic side? Driven by this question, Rob Sears began combing Trump’s words for signs of poetry.What he found was a revelation. By simply taking the 45th President of the United States’ tweets and transcripts, cutting them up and reordering them, Sears unearthed a trove [More]
(as of April 19, 2020 1:00 pm GMT+0000 - Details) + Add To Wish List
(as of April 20, 2020 5:01 am GMT+0000 - Details) + Add To Wish List
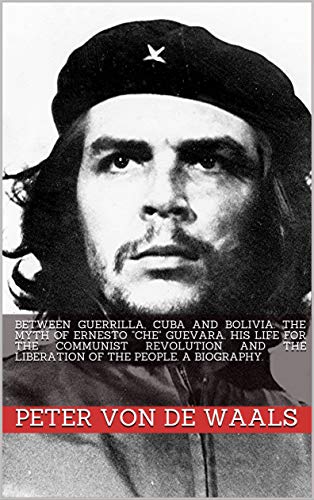
On the trail of a mythErnesto Che Guevara is one of the most formative, but also one of the most controversial historical figures of the 20th century. Thus Holtz described Che Guevara as “a Trotskyist, a Maoist, a Marxist heretic, a Communist Robin Hood, a red pyromaniac, an anarchist and militant dreamer, a radical left-wing [More]
(as of April 20, 2020 5:01 am GMT+0000 - Details) + Add To Wish List